shoulder anatomy
Shoulder pain can develop after an injury, overuse, or from degenerative changes. It is often difficult to relate the onset of shoulder pain to a particular event which makes diagnosis of the problem more difficult. The key in relieving shoulder pain is prompt diagnosis and treatment.
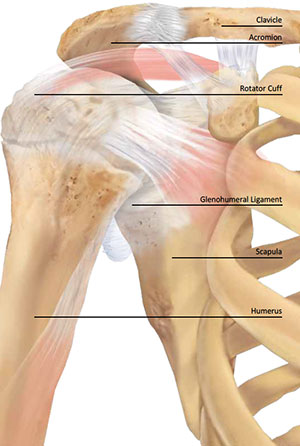
Most traumatic shoulder injuries in the elderly can be classified into two groups: fractures of the humerus (arm bone) and tears of the rotator cuff (the group of four tendons that surround the shoulder and allow for normal motion).
After a fall, the shoulder is normally sore and there is significant pain with motion of the shoulder. An x-ray or, less commonly, a CAT scan is used to diagnose a fracture. If the fracture is non-displaced (the bones are well lined-up), usually a sling is all that is needed and the prognosis for full recovery is excellent. If the fracture is displaced (not lined-up) then prompt intervention is required. This may include setting of the bones in the emergency room or a trip to the operating room for realignment and possible placement of hardware (screws, plates, rods, or nails) to maintain the alignment. The prognosis for recovery and return of function will depend on the severity of the break and the procedure needed to fix it.
Shoulder soreness and an inability to raise the arm may indicate a torn rotator cuff. These tears can occur by themselves or in combination with a fracture or dislocation (popping out of joint) of the shoulder. A torn rotator cuff is diagnosed on physical examination and with MRI scanning. The torn end of the tendon (or tendons) can be seen retracted away from the bone to which it was previously attached. We use the MRI to predict outcome and the need for surgical repair of the torn tendon. The repair can be done open (an incision is made), mini-open (a small incision is made combined with part of the procedure done arthroscopically), or all arthroscopically (minimally-invasive surgery using a camera through punctures around the shoulder). The less-invasive procedures allow for easier and faster rehabilitation of the shoulder. The prognosis after rotator cuff repair (regardless of the repair method) is good for pain relief and return of function. This will vary according to the size and chronicity (how old is the tear) of the tear.
Most overuse-type shoulder problems are caused by tendonitis. Most-commonly, the rotator cuff is involved, though the biceps and deltoid tendons can also be affected. Tendonitis is an inflammation (and even partial tearing) of the tendon which causes pain when the muscle is used. Rotator cuff tendonitis is usually due to an abrasive bone spur in the shoulder or a calcium deposit and most patients have pain with overhead activities and pain at night. Cortisone injections, anti-inflammatory medication, and physical therapy can often relieve the symptoms. If relief is temporary or incomplete, arthroscopic surgery can be performed to remove the bone spur or calcium deposit. The prognosis for full recovery after treatment is excellent.
Degenerative changes in the shoulder can affect the rotator cuff tendons, the glenohumeral joint (ball-and-socket of the shoulder), and the AC joint (end of the collar bone). With continued wear-and-tear on the shoulder, the cartilage in the joint can deteriorate leading to arthritis. AC joint arthritis can be treated with a cortisone injection or a small arthroscopic or open procedure to remove the very end of the collar bone. There is an excellent prognosis for relief of pain and return of function. Degeneration of the rotator cuff tendons can be treated with therapy, debridement of the tendon, or repair of the tendon. The prognosis will vary according to the degree of degeneration. Pain usually resolves but there may be some residual loss of function.
Degeneration of the ball-and-socket joint can be the most debilitating but is also the rarest. When arthritis of the shoulder becomes severe, the patient often has pain with use of the arm, a significant loss of motion in the shoulder, painful cracking or popping in the shoulder, and severe pain at night. Diagnosis can usually be made with a physical examination and an x-ray. Often, a cortisone injection and some activity modification will greatly improve the pain but the motion loss will not improve. Eventually, a total shoulder replacement may be necessary. This operation replaces the ball with metal and the socket with plastic. This provides significant pain relief and improvement in motion and function of the shoulder.
In conclusion, diagnosis of shoulder problems is often difficult requiring careful examination and imaging studies. Prompt treatment for most conditions will best assure relief of pain and a return to an active lifestyle.
